Recently, the Indian state of Kerala has seen 2 deaths due to the said outbreak of Nipah Virus. The total known caseload on 15 September has touched a mark of 6 active cases. The government authorities including Kerala State Government and Indian Central Government have come into action to prevent a strong outbreak of the disease.
Containment Zones have been created, Schools have been shut down, and lockdown type of measures are in place to counter the outbreak in the initial stage only. The teams of the virology experts have been studying the cause of the outbreak.
Though the virus is less transmissible than the SAARS Covid-19, its fatality rates are high, raising concern among people and authorities. In this article, we will discuss Nipah Virus, the concerns associated and Safety Measures.
Nipah Virus
Nipah virus is a zoonotic virus. The organism that causes Nipah Virus encephalitis is an RNA or Ribonucleic acid virus of the family Paramyxoviridae, genus Henipavirus, and is closely related to Hendra virus.
It was first identified in Malaysia and Singapore in 1998 and 1998 during an outbreak among pig farmers, and subsequent outbreaks have occurred in South and Southeast Asia. The disease is named after a village in Malaysia, Sungai Nipah, where it was first detected.
Nipah virus is primarily transmitted from animals to humans, with fruit bats serving as the natural reason for the infection. An individual coming in contact with any body fluid of an infected or dead bat by any means starts the chain of infection from bats to humans and then humans to humans, through close contact which makes it a significant public health concern.
The symptoms of Nipah virus infection can range from mild respiratory issues to severe encephalitis, reflected in the body of an individual by fever, headache, drowsiness, and confusion. Unfortunately, there is no specific antiviral treatment for the Nipah virus, which makes prevention of the disease very easy.
Concerns Related To Nipah Virus Infection
Nipah virus infection raises a significant number of concerns for individuals and public health authorities. The Nipah Virus has been responsible for outbreaks with high morbidity and mortality rates.
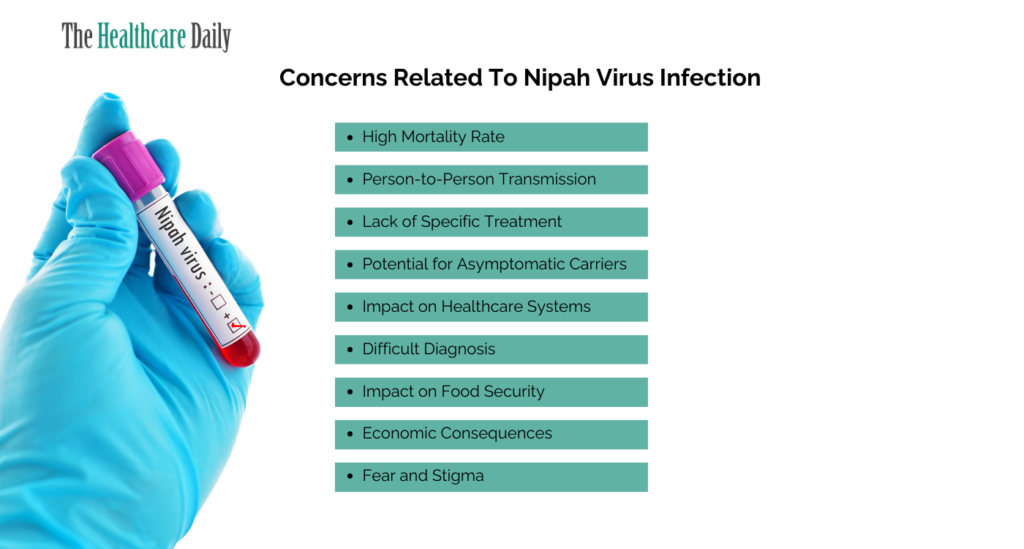
High Mortality Rate:
One of the most significant concerns associated with Nipah virus infection is its high mortality rate. In some outbreaks, the fatality rate has exceeded 70% which makes it a deadly pathogen. This high mortality rate intensifies the fear and concern surrounding Nipah virus outbreaks.
Person-to-Person Transmission:
Unlike some other zoonotic diseases, the Nipah virus has the ability to spread from person to person. This person-to-person transmission increases the risk of strong outbreaks in densely populated places. And, containing such outbreaks is a huge challenge for healthcare systems and authorities.
Lack of Specific Treatment:
Nipah virus doesn’t have an antiviral treatment or vaccine approved for human use. This unavailability of treatment leaves patients with very limited options to manage the infection once contracted. The absence of effective treatments heightens concerns about the ability to provide adequate care during outbreaks.
Difficult Diagnosis:
Diagnosing Nipah virus infection is a challenging task in the early stages when symptoms resemble those of other common illnesses like influenza or dengue fever. This difficulty in early detection can lead to delays in implementing containment measures which allows the virus to spread.
Potential for Asymptomatic Carriers:
Some individuals infected with the Nipah virus remain asymptomatic or have mild symptoms which makes it hard to identify and isolate cases effectively. These asymptomatic carriers can contribute to the transmission of the virus, further complicating outbreak control efforts.
Impact on Healthcare Systems:
Nipah virus outbreaks can place immense stress on healthcare systems in resource-limited areas. The need for isolation facilities, specialized equipment, and trained healthcare personnel overwhelm local healthcare infrastructure which leads to concerns about the overall capacity to manage outbreaks effectively.
Fear and Stigma:
Communities affected by outbreaks can face discrimination, which hinders cooperation with containment efforts placed by the government authorities. Fear can also lead to delays in seeking medical care, potentially worsening the outcome for infected individuals.
Economic Consequences:
Nipah virus outbreaks can have many economic repercussions in regions where agriculture and farming are key professions. Killing livestock, like pigs, to prevent further transmission result in financial losses for farmers and disrupt the local economy.
Impact on Food Security:
Nipah virus is linked to the consumption of raw date palm sap contaminated with bat excretions. This has raised concerns about food security and the need for safer food handling practices in areas where such consumption is common. Balancing cultural practices with the need for food safety remains a challenge.
Safety Measures During Nipah Outbreak
In regions where the Nipah virus is active, taking strict safety measures is mandatory to protect yourself and your community. Outbreaks can be devastating but with the right precautions, the risk of transmission can be significantly reduced.
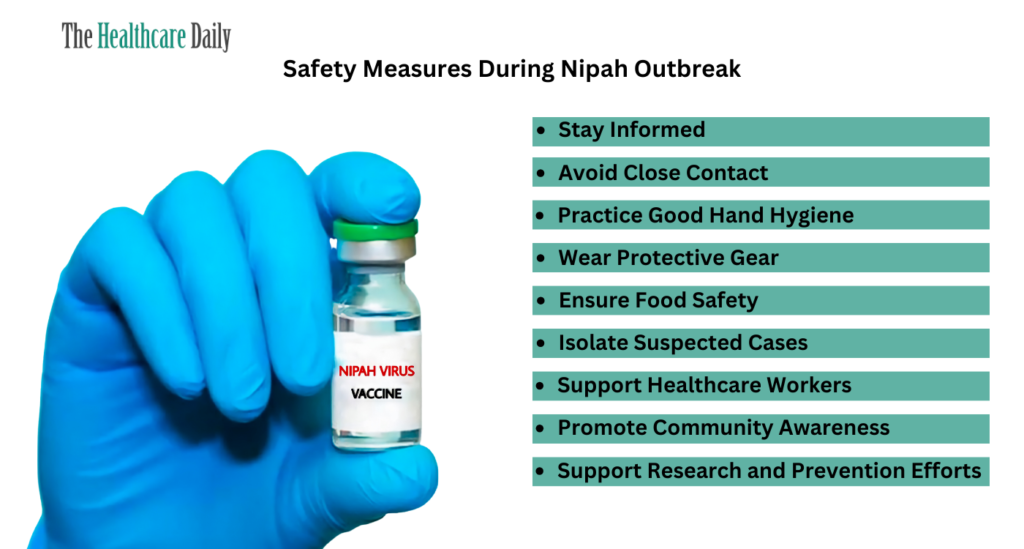
Stay Informed:
Knowledge is your best defence. Stay updated with official information from local health authorities, the World Health Organization (WHO), and the Centers for Disease Control and Prevention (CDC). This includes being aware of the current situation, transmission patterns, and recommended safety guidelines.
Avoid Close Contact:
The Nipah virus spreads from person to person via direct contact with infected individuals. Strictly maintain a safe distance (at least 1 meter or 3 feet) from anyone showing symptoms of Nipah virus infection, such as fever, cough, and difficulty breathing. Avoid hugging, kissing, or shaking hands with them.
Practice Good Hand Hygiene:
Wash your hands regularly with soap and water for at least 20 seconds after touching potentially contaminated surfaces or coming into contact with someone who may be infected. If soap and water are not available then use an alcohol-based hand sanitizer with at least 60% alcohol content.
Wear Protective Gear:
If you are caring for someone with suspected or confirmed Nipah virus infection then use appropriate personal protective equipment (PPE). It may include gloves, masks, gowns, and eye protection gear. Follow proper procedures for putting on and removing PPE to prevent self-contamination.
Ensure Food Safety:
Practice food safety measures thoroughly. Cook all meat properly, especially pork, as the virus can be present in the tissues of infected animals. Avoid consuming fruits or vegetables that may have come into contact with contaminated bat excretions.
Isolate Suspected Cases:
If you or someone you know is showing symptoms consistent with Nipah virus infection then seek medical attention immediately. Isolate the individual to prevent potential transmission to others while awaiting diagnosis and guidance from healthcare professionals.
Support Healthcare Workers:
Healthcare workers are on the front lines during outbreaks. You should respect and follow their guidance, and comply with any quarantine or isolation measures which they recommend. This helps protect both you and those working tirelessly around the clock to contain the virus.
Promote Community Awareness:
Educate your community about the Nipah virus and the importance of safety measures. Encourage others to follow guidelines, report suspected cases promptly, and cooperate with health authorities.
Avoid Unnecessary Travel:
During active Nipah virus outbreaks, consider limiting non-essential travel to the areas with confirmed cases. Travel increases the risk of exposure and transmission.
Maintain Good Respiratory Hygiene:
Cover your mouth and nose with a tissue or your elbow when you cough or sneeze. Dispose of used tissues properly and wash your hands immediately.
Support Research and Prevention Efforts:
Researchers are continually working to better understand the Nipah virus and develop treatments and vaccines. Support and participate in research studies and clinical trials when possible.
Conclusion
In conclusion, the outbreak of the Nipah virus raises grave concerns for individuals and communities. The recent cases in Kerala serve as a stark reminder of the virus’s potential threat. With a high mortality rate, person-to-person transmission, and no specific treatment, Nipah virus outbreaks demand strong vigilance and collective action.
Effective containment measures, including isolation, school closures, and lockdowns, are essential in the early stages of an outbreak. However, the challenges posed by the Nipah virus go beyond healthcare. Fear, stigma, economic consequences, and impacts on food security are all significant issues that communities must grapple with during an outbreak.
Nonetheless, knowledge and awareness can empower individuals and communities to mitigate these concerns. Staying informed, practising good hygiene, and supporting healthcare workers are crucial steps in curbing the virus’s spread. By adhering to the guidelines and working together, we can navigate the challenges posed by Nipah virus outbreaks and protect the health and well-being of our communities.