In a breakthrough study, researchers at Lund University in Sweden have developed a completely unique Bioink that permits human airway passages to be bio-printed using the host’s cells.
The 3D-printed structures use a biocompatible material that supports the expansion of the latest blood vessels inside the transplanted organs. This might be the primary step toward the 3D printing of organs.
Organ printing is sort of almost like the traditional way of printing papers. Here a computer model of the organ is entered and therefore the printer lays down successive layers of biocompatible wax or plastic. The plastic holds the organ because of the scaffolding material.
During the event, this is often seeded with the host cells in order that the organ doesn’t get rejected by the body. This is often being developed to ease the organ transplantation process and also its potential impact on pharmaceutical industries.
Chronic lung infections are the third commonest explanation for death around the world. there’s not any particular treatment for these sorts of diseases as of now. Only lung transplants could help terminally ill patients, but still, there aren’t enough donors to satisfy this clinical demand.
So researchers around the globe try to seek out ways during which enough donor lungs might be made. a method is to fabricate the lung tissues by combining a number of the cells to a scaffold that’s bioengineered.
“We started small by joining small tubes because this is often a feature found in both airways and within the vasculature of the lung.
By using our new bioink with stem cells isolated from patient airways, we were ready to print small airways which had multiple layers of cells and remained open over time”, explains Darcy Wagner, professor and senior author of the study.
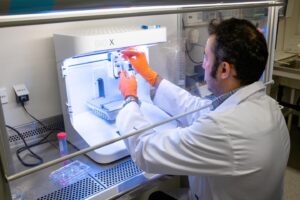
The researchers first composed a replacement bioink for 3D-bioprinting human tissue. The bioink was made by combining two materials: a cloth derived from seaweed, alginate, and an extracellular matrix derived from lung tissue. The Bioink was tested on how it supports the bioprinted structures towards its development to make tissues.
Then the ink was wont to create airway passages using two sorts of cells found within the passage. However, this ink isn’t particularly developed for lung tissues, but it is often adapted to make different cells and tissues also.
The author of the study also admitted that there’s space for further technological developments within the available bioprinters in order that larger and more distal tissues might be made with higher resolution.
“The development of this new bioink will be a significant invention, but it’s important to further validate the working ability of the tiny airways over time and to explore if this approach could be used in large animal models”, concludes Martina De Santis, the primary author of the study.